Let’s say it like it is. You’ve cut carbs, said no to dessert, worked out five days a week and still, the lower belly pouch won’t budge. You might’ve even asked your doctor about it, and got a vague answer: “It’s probably hormonal.” End of story.
But here’s the thing: they weren’t wrong, just… incomplete.
This is not medical advice, just an awareness message. So you do your own research and talk to your physical first. The kind of terms doctors don’t always have the time to unpack.
So the hormone is called cortisol.
Your Body’s Built-In Survival Alarm
It is a stress hormone produced by your adrenal glands. It’s actually useful because it helps you wake up, manage energy, and respond to pressure. But when cortisol stays elevated for long periods (because of work stress, poor sleep, under-eating, or even over-exercising), your body starts to hold on to fat—especially around your midsection. Here’s a breakdown of how cortisol affects belly fat and why it becomes so stubborn.
Where?
Right around your waistline.
Why there? Because belly fat is metabolically active and easily accessible fuel. It’s your body’s emergency ration like a pantry it doesn’t want to empty.
Here’s what your doctor probably didn’t explain fully: It doesn’t just mess with your fat storage, it affects hunger, sleep, cravings, mood, even your motivation to move.
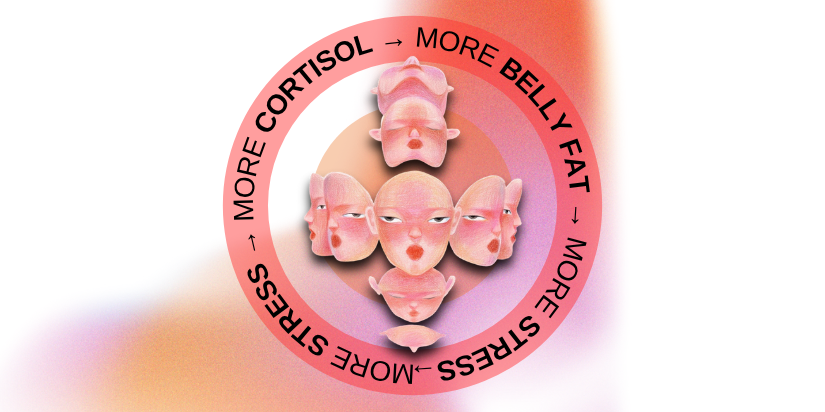
And all of this becomes a feedback loop.
Might Be Creeping Up on You
This isn’t just anecdotal. Research points to a stress-induced cortisol response and fat distribution in women, which shows how emotional and physical stress can quite literally reshape how your body stores fat. Without turning this into a medical checklist, let’s look at common signs women often notice:
A lower belly pouch that won’t go away, even with dieting
Mid-day crashes or irritability
Cravings for salty or sugary foods in the evening
Trouble sleeping (you feel tired but wired)
A “thicker” midsection that feels inflamed, not just soft
Sound familiar? It’s not in your head. It’s likely due to your hormones.
Food as Your First Line of Calm (Not Control)
We’ve all read those lists: “Eat these 5 foods to lose belly fat.” But cortisol doesn’t respond to restriction—it responds to nourishment. What actually helps is balancing your blood sugar and lowering internal stress with nutrients that support hormone regulation.

These aren’t diet tricks. These are your body’s tools to feel safe again.
So Why Didn’t Your Doctor Tell You This?
It’s not about secrecy or bad intentions. Medical training is designed to diagnose illness not always to decode discomfort. Unless your stress hormone levels are drastically off, they often don’t make it into the conversation. But that doesn’t mean the symptoms you feel are any less real.
Many women today live in the “in-between” zone, not technically unwell, but far from feeling balanced. That constant bloating, the unexplained belly fat, the foggy headspace it’s not a clinical emergency. But it is your body speaking up.
That’s where resources like this step in to bridge the gap between data and daily life. To translate the missing pieces your appointments might not cover.
What to Start Noticing
No crash diets. No supplement overload. Just simple, body-aware shifts that support hormonal calm:
- Create daily moments of pause: That constant go-go-go mode isn’t a badge of honor. It keeps your stress response activated longer than it needs to be.
- Eat with rhythm: Skipping meals or over-restricting might feel productive, but it can confuse your metabolism and increase stress internally especially for women.
- Add omega-3s: Think flax, walnuts, chia seeds. These do more than boost skin glow; they help support emotional and hormonal resilience.
- Tune into your signals: Does that evening snack soothe your nerves more than your hunger? Your nervous system might be seeking grounding, not calories.
What Your Body Has Been Trying to Tell You
That belly weight you’re noticing may not just be “fluff.” It could be linked to something deeper—like visceral fat and its connection to cortisol, which is metabolically active and more than just a cosmetic concern.
If you’ve been feeling like something’s off but your labs are “normal” and your doctor says you’re fine, trust that your body might be speaking a different language.

Understanding the cortisol belly fat link isn’t about fear. It’s about finally giving a name to something you’ve felt for a while. And once you name it, you can start working with your body instead of punishing it.
No guilt. No guesswork. Just awareness.